(Note from Shelley) Body Mass Index is a calculation based on your height and your weight. It’s supposed to be a way to determine whether you’re thin or fat. A bigger BMI, has not been considered healthy. Earlier this year, that got challenged, when the Journal of the American Medical Association published a study that looked at their BMI and death rates. Their conclusion – basically, people with a higher BMI tended to live longer. Dr. Ron Rosedale says that’s beside the point. The bigger issue is that using BMI as a measure for health is Bunk.
FULL TRANSCRIPT (Paraphrased)
RON ROSEDALE: The study from the Journal of the American Medical Association (JAMA) about BMI is not a new study, and it is not new information at all, but has been rehashed in the medical community extensively. For example, here’s a study that was first published in the British Medical Journal, the Lancet in 2006. The 2006 study is titled, “Association of Body Weight with Total Mortality and Cardiovascular Disease. A systematic review of cohort studies.” In other words, the 2006 study is about virtually the same topic as the new one from JAMA, except the Lancet study was done in 2006.
Both JAMA and the Lancet are highly regarded journals. Did they reach the same conclusions?
RON ROSEDALE: Their research findings were the same, but their conclusions were different. The 2006 Lancet findings, and I’ll just quote the study, were this: “We found 40 studies with 150 to 250 patients, with a mean followup of three to eight years.” In other words, the researchers in 2006 used basically the same statistical criteria as the current study in JAMA. The 2006 version was a retrospective study that kind of compiled a bunch of other studies – as did the current JAMA study. And after compiling the data, the Lancet researchers looked at relative risk of BMI as a marker of obesity. Just as in the JAMA study, in the 2006 Lancet study, the data showed that people with a low body mass index, in other words . . . skinny people . . . had an increased relative risk of mortality.
In the Lancet study, if you were skinnier than most people at the beginning of the study, then to three to eight years later, you were more likely to be dead!
RON ROSEDALE: Correct, which is what the current JAMA group found as well. Also like the current study, the Lancet study found that people who are overweight, as indicated by a BMI of between 25 and 29.9, had the lowest risk for total mortality and cardiovascular mortality, compared to people with a normal BMI. Obese patients, those with a BMI between 30 and 35 had no increased risk for total mortality. Patients with severe obesity, in other words, a BMI greater than 35, did not have an increased risk for overall mortality. But they had the highest risk of cardiovascular mortality. The findings in this 2006 study were almost identical to the findings in the current JAMA study.
But even though the 2006 Lancet findings were similar to the JAMA current study, you say there’s a major difference? What was it?
RON ROSEDALE: The biggest difference between then and now is the interpretation of the BMI data. For the 2006 Lancet study, this is the conclusion, right off the bat. And I quote:
“The better outcome for cardiovascular and total mortality seen in the overweight and mildly obese groups, could not be explained by adjustment for confounding factors. These findings could be explained by the lack of discriminatory power in the ability of BMI to distinguish between body fat and lean body mass.” (THE LANCET, 2006)
RON ROSEDALE: The 2006 Lancet study’s conclusion is correct. BMI’s a bad way to measure health or disease. The current JAMA study doesn’t say this. It left saying something about that to an editorial in JAMA. But the lack of relevancy to health, in measuring BMI, was already mentioned by the authors of the 2006 study. In other words, back in 2006, they already had realized that having a higher BMI, that is, being fat, is not protective in and of itself. What the 2006 showed, and correctly concluded, is that using body mass index as an index of obesity is faulty. After that 2006 study in Lancet, and other similar studies, there were a number of articles and studies that talked about BMI not being a valid measure of obesity, and why it should be dropped altogether, and that one should use more valid measures of health and obesity, such as just measuring your waist circumference or better yet, your waist to hip ratio. Back around 2006, switching from measuring BMI to measuring waist to hip ratio was widely discussed in the medical literature. So why, in the current issue of JAMA, they’re going back to studies using BMI, and making it into a big news story, is to me an indication of a major disease in medicine itself. The disease is that medicine hates change. It seems that medicine would rather allow people to continue to get faulty information and continue to get unhealthy and even continue to die, rather than admit that they made a mistake, for decades. The mistake here in the U-S is that they’re still using BMI as if it’s a valid measure of health.
Is BMI the Arnold Swarchenegger paradox? That is, muscles weigh more than fat, and in his prime, we was full of muscles. Heavy. Based on his height and the bathroom scales, his BMI was over 30 – obese – but really was just full of muscle.
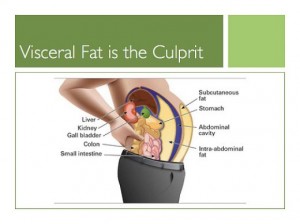
RON ROSEDALE: That’s part of it. BMI doesn’t differentiate between between muscle and fat. Certain athletes will have a higher BMI than what has historically been considered healthy. But even more important, BMI doesn’t differentiate between where that fat is. If the fat is subcutaneous, creating a pear shaped body, for instance, that fat is not a health issue. You know, the shape when women put fat on their hips.
Subcutaneous. That means the fat’s just under your skin, but above your muscle.
RON ROSEDALE: Right. It’s not visceral, meaning belly fat. Belly fat’s a sign of health problems.
When you say, belly fat, you’re not talking about the fat that you could grab, right under your skin. You’re talking about the belly fat that would be inside of your body, underneath the muscle, surrounding your body organs.
RON ROSEDALE: Yes surrounding the viscera, which means the body organs, and as a special problem for health, the fat that’s surrounding and permeating the liver.
Is this the kind of fat in a man, for instance, who has a barrel shaped tummy that looks fat. But if you pat that tummy, it stronger and harder than you might expect, because a lot of it is under the stomach muscles – surrounding the body organs.
RON ROSEDALE: That’s correct, and it’s been shown very convincingly, that when one has significant visceral fat, especially liver fat, which is called fatty liver, then it’s a powerful risk factor. Although it’s called a risk factor, it’s actually a disease itself. It indicates your body is failing to understand where to put the fat. So, it puts the fat in all the wrong places. Whereas, if you were to accumulate excess fat, it’s advantageous, in some cases, to store food energy as fat. In our ancestral history, it was quite important to store extra energy in the form of fat, when food was abundant so you could call on those energy reserves when food was scarce. Another example is bears who hibernate eat a lot in the fall, they eat a lot of berries, and they get fat, and it’s subcutaneous fat. And they can then call on that fat while they’re hibernating, and they have a very low incidence of cardiovascular disease, so that type of fat does not cause disease.
Ron Rosedale, are you saying that someone could have a fairly high amount of body fat. But, if it’s stored on the hips, or if it’s stored on other parts of the body where it’s above the muscle layer, just below the skin, it’s probably not going to be a health problem. Or at least, not as much of one.
RON ROSEDALE: That’s correct. Because it actually indicates the body knows what it’s doing. That’s where one is supposed to store fat, underneath the skin, when you have energy in abundance. That’s a safe place to store it. It doesn’t do harm there. And really, fat below the skin is actually a different organ than fat under the muscle and around the body organs. If you want to look at it from a physiological sense, we know now that there are different kinds of fat. There’s brown fat, which is thermogenic and emits a large amount of heat. Humans have it to a fairly small extent. Rodents have it to a larger extent. But the fat that’s in the viscera is a different kind of fat than the fat that’s subcutaneous. The fat that’s in the viscera produces a lot more hormones and inflammatory hormones, There’s a lot of talk and study and rightly so, about the contribution of chronic inflammation to chronic disease. And a lot of that chronic inflammation is initiated by fat, which is initiated by high levels of a very powerful metabolic hormone called leptin. We know that when leptin is not being signaled properly, the brain ceases to understand that the body has an appropriate amount of fat and then it actually thinks you’re too skinny, and it causes you to be hungry, so you eat more and you store more fat for potential times of famine and need, even though you actually have a lot of fat. There’s a disconnect between the body and the brain but more important, we know that when there’s that disconnect, and the brain can’t hear the leptin signal, the more devastating result of this is not just that the person gets fat, but gets fat in the wrong places. Such as visceral fat which produces a lot of inflammation, then you get into a vicious cycle that perpetuates disease.
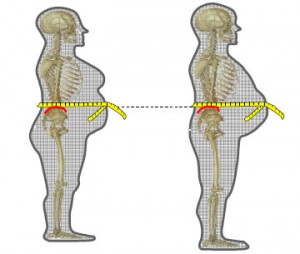
If visceral is the dangerous kind of fat, and subcutaneous is not, you mentioned measuring your waist to hip ratio is one clue about whether or not you’re in the safe zone when it comes to your fat. Is there a ball park ratio to look at, between your waist and your hips?
RON ROSEDALE: Yes. What’s interesting about the current article is that it’s not new. That they’re still talking about BMI as a useful marker for obesity, even though it has been shown, very convincingly, as a really poor marker. So, going back to studies from earlier that poo-pooed BMI as a valid marker for obesity. They started using waist circumference and waist to hip ratio, and so there have been some standards that have been set up. For men, a ratio of above 1 is considered to be a higher risk of more visceral fat, and therefor more risk for disease.
For men that means that if your waist is no bigger than your hips, you’re probably in a good place, and where exactly should you measure that? Should you measure that at a bikini line or right at your navel?
RON ROSEDALE: The largest circumference.
Uh-oh. Instead of saying, well, I’m going to put the tape measure where my belt fits the best underneath my belly, measure the biggest part.
RON ROSEDALE: Measure at the biggest part of the belly and the biggest part of the hip. And for women, it should be .8.
The waist should be 80% the size of the hips, or less. And where should women measure that? Above the belly, or below the belly where the abdomen pooches out the most?
RON ROSEDALE: I think it should be measured where the abdomen is the greatest and the hips are largest as well.
So don’t just measure up above or below the belly. Just go ahead and admit, this is where I’m the biggest, and measure there.
RON ROSEDALE: That’s correct.
That’s so unfortunate. That’s going to put so many people’s waist to hip assumptions into a less flattering light.
RON ROSEDALE: That’s correct. But the truth is never bad. You have to use the truth, especially when it comes to health.
The truth may not be ever bad, but it can be disconcerting.
RON ROSEDALE: Well, it can. If it is viewed that way. But a different perception is to view the the truth as causing the freedom to make appropriate changes. You have to know that there’s a problem first, before you make a change.
So we’ve been talking about the side of how to determine whether your body fat is in a safe place and in a safe amount. But what about the other side of this study that said that people who are thin are more likely to die? That implies that right now, after the holidays, when many people have put on a little weight Instead of trying to get down to a thinner weight, they should celebrate that they’re more pleasingly plump.
RON ROSEDALE: I think that the entire study needs to be thrown away, because it uses an invalid measure of obesity, which is BMI. The study itself, and any conclusions that one can draw from it, are irrelevant. That’s all I can really say about this particular study. It doesn’t show that being skinny is beneficial or harmful. It doesn’t say anything. That being said, I wouldn’t say that being particularly skinny is advantageous. It certainly wasn’t advantageous to our ancestors, where if a skinny person encountered a famine, which was an almost certainty at some point, a person would have less chance of surviving. The endeavor to have 8% body fat, as in a marathon runner, is a very poor endeavor for health. Over exercising is quite common, actually. This country has far more health clubs per capita than any other country on earth, and yet it’s not reflected in our health. It’s really very hard to find even animal studies to show that increasing exercise promotes longevity. You have to look deeper. You have to look at what is actually controlling the fat. You have to look at the metabolic hormones. You have to look at the communication. I think we’ve said relatively frequently on this show that health is going to be determined by the communication of 15 trillion cells so that they can act collectively and harmoniously as one. Disease and health are going to be determined by the communication between the different cells. The majority of that communication is going to be mediated by the hormones. Of those hormones, the ones that regulate metabolism to me, are the most important. Metabolism can be defined as the biochemical reactions that turn food into life. That’s extremely important. And when you have proper metabolic chemistry you will continue to live in a healthy manner, as much as possible.
Can someone have proper metabolic signaling and be thin or be fat, and be healthy as long as their metabolic signaling is good?
RON ROSEDALE: Yes.
When you look at someone and they look like a model from Shape Magazine, or you look at a weight lifter who is also a runner, or you look at someone who’s the size of Oprah Winfrey, you say any of those people could be healthy, but you need to look deeper?
RON ROSEDALE: That’s correct. They could be healthy. They might not. There are certain factors one could look at and guess that they’re not as healthy. Certainly in the overly obese, or people who are obviously apple-shaped, you can pretty much guess that their metabolic hormones are out of whack, or they wouldn’t be storing so much belly fat. The harder determination would be to look at people who are relatively skinny. Because we know that skinny people can be insulin resistant. We know that skinny people can have diabetes. Certainly lots and lots of skinny people have died of heart attacks. Many runners have died of heart attacks. Many skinny people will acquire cancer. And once heavy people have cancer, they will become skinny.
If someone today has TB, or AIDS, if they die of the disease three to eight years later, are they likely to be skinny or fat when they die?
RON ROSEDALE: Almost any sickness will cause a person to essentially start disappearing. Their life is basically being sucked out of them.
Did this study take into account those kind of chronic and deadly diseases.
RON ROSEDALE: No. They just looked at BMI. I’m not sure the real purpose of the study. The same question made headlines in 2005 and 2006. At that time, the researchers looked at the studies that correlated BMI and with mortality and pretty much concluded that it wasn’t the obesity that lent a protective effect. It was simply that BMI is an invalid marker of health problems due to obesity. Yet here again, six years later, they do it again. I don’t understand it. But you see that so often in medicine. They have such a hard time letting go of paradigms. Look at cholesterol. This cholesterol myth has been going on for half a century. That’s a devastating myth that keeps being perpetuated because there’s so much money behind it. All the cholesterol drugs. More and more studies are coming out about the adverse effects of cholesterol lowering, and especially lowering cholesterol with drugs. And yet, they continue to hang onto it. You see the same thing with taking calcium for instance, and we’ve done interviews on the detriments of taking calcium. You see the same thing in the adage that eating fat makes you fat. There are just so many myths in medicine that continue on and on.
You feel like they have put a lot of time and money into something that’s not worth analyzing anyway.
RON ROSEDALE: It’s already been analyzed. It would not be such an issue, except that it had already been looked at over a decade ago, and been scrutinized over by many experts who concluded that BMI is not a great measure of obesity. And yet, the standard medical community continues to come out with stuff like this that add to people’s confusion and causes far more harm than good.
Instead of stepping on the scales and using that as a major marker for health, people might be better off if they get out a tape measure. Measure the widest part of their belly, tummy or abdomen and then measure the widest part of their hips. For men, waist to hips should be around 1:1. For women, waist to hips should be .8 to 1 or less. And that would be a better way to tell how their health is doing.
RON ROSEDALE: That would be a far better measure than BMI. And then one can go a step further and understand what actually controls their waist to hip ratio. These would be metabolic hormones. A person can easily have their leptin measured. It’s not routinely done. They’ll go and have their cholesterol measured instead. Yet, leptin is a far more significant factor in future health risks. How well the body is able to listen to leptin, as shown by just a fasting leptin level. Very simple to do, and no harder than checking cholesterol. And not much more expensive.
So you’d rather have leptin be a standard measure.
RON ROSEDALE: It should be done in everybody. There’s so much science now that shows the critical importance of leptin. In a roundabout way, this study supports that, too. The study shows that it isn’t just obesity that matters. Even if BMI was correct, it’s how you get fat that matters. Let’s say that this study is correct, and that BMI is valid, neither of which is true, but let’s say, for the moment that they are. Even this study shows that it’s not obesity that causes disease. It’s something else. It’s not the fact that you were overweight or obese, but how you got there. Did you get there because your leptin wasn’t being heard properly, or you’re insulin wasn’t heard properly? Then you’re in trouble. If you got there just because you overate and it got stored appropriately, without leptin or insulin being impacted then you’re probably not going to be in harm’s way, so much.
Let’s look at this idea of testing leptin. When’s the right time of day to measure it, and does it vary depending on what you’ve eaten and when you ate? The reason I’m wondering is that insulin varies a lot, depending on what you eat. For some people, their level of insulin is normal as long as they haven’t eaten in 12 hours. But a small percentage of people, if they piece of bread, or they drink a soda, their blood sugars stay fairly normal, but their insulin level may go sky high. So for some people, they can learn extra stuff about about how their body responds if they start with a fasting insulin level, then eat something, and then track their insulin levels and sugar levels for the next 2 to 5 hours. In other words, eating reveals what’s happening with their insulin more than just doing a fasting test without eating anything. Is leptin similar? Is it useful to see how eating affects its ups and downs. Or, is it just enough to check for a fasting leptin level?
RON ROSEDALE: Like insulin, leptin varies by what you eat. Perhaps not as dramatically, and as quickly, as insulin, which generally starts to change within minutes and a few hours, based on what you eat. Leptin’s response is slower. But within 12 hours, leptin will also go up 50% or so, depending on what you ate. But it isn’t just so much the short-term, after meal levels of these hormones. It’s the long-term impact. If your levels of leptin and insulin continue to go high. If they continue to spike after weeks and months and years and decades of a high carbohydrate diet, that is known to increase insulin and leptin. By constantly increasing the levels of these hormones, it deadens the cell’s ability to listen to these hormones. Kind of like being in a smelly room. If you stay in that room, you can’t smell it anymore. As cells are constantly flooded by high levels of insulin and leptin, over time, years and decades perhaps, they cease to hear the instructions of those hormones, even at high volume, so that previously, for instance, a relatively low level of leptin would signal the brain to say that you’ve got enough fat stores and you can stop being hungry and you should stop eating more, and over time, the hypothalamus in the brain, which is a very critical area, it can’t hear the message any more. So it no longer stops being hungry. It no longer sends messages the signal you to stop feeling hungry so you can stop getting fatter It tells you to be hungry and stop burning the fat that you’ve got, which is a faulty message. So those constant spikes lead to hormonal resistance. It leads to leptin resistance and insulin resistance. These accelerate the rate of aging. It’s a complex and vicious cycle, but you can have a pretty good idea of someone’s level of insulin or leptin resistance just by doing a fasting test of those hormones.
You can even order those tests on line these days. I just looked on line, and you can order an insulin test for between $30 and $80. You can order a leptin test for $100 to $180. So if a doctor doesn’t want to order the test, you can anyway! A simple fasting insulin and leptin test would help someone know more about how their body fat, and the foods they eat, are helping or hurting their health. But with insulin, you can also do an after-meal test, that can help some people who have normal insulin levels most of the time, discover that they can get a huge spike of insulin within an hour or so of a meal. But what if you wanted to know if you had a hidden problem with leptin spikes?
RON ROSEDALE: You’d probably have to weight eight to 12 hours after you ate, and it’s hard to do it exactly at the right time. With insulin, you can give someone some food, or some sugar, and in the next 2 to 5 hours, test the response in the office. It’s more difficult to do with leptin, so it’s not done. You know, though, I started talking about the importance of leptin maybe eight years ago. Even a fasting leptin test is a rare one. Fasting insulin isn’t being done routinely in most doctor’s offices, but at least it’s being thought about and talked about. It takes so long for medicine to advance, and especially when it entails an about face from previous recommendations. They like to stick with old recommendations for such a long time, in part, I suppose, because if you do what everyone else is doing, you don’t get in trouble. After all, doctors don’t want to get sued.
RON ROSEDALE: If a person wanted to go to that trouble and expense, it would certainly be fine to me, but you have to look at the underlying cause. If you found out you had fatty liver, you still have to figure out what’s causing it. when someone has a diagnosis of fatty liver disease, you need to narrow down to a problem of communication, and a problem of communication of hormones. So you’d still have to look at leptin and insulin. So why not just start there?
It sounds so simple that way.
RON ROSEDALE: It is simple. It really behooves people to take control of their own health. Unfortunately the medical profession is under control of large corporations that really don’t have health as their priority.
Are you a thin person or a fat person?
RON ROSEDALE: I have a medium build, I suppose.
Do you carry a tape measure in your pocket?
RON ROSEDALE: (LAUGHS) No, I don’t. But when I was in practice, we were measuring waist to hip ratios.
But BMI is less embarrassing to measure than using a tape measure.
RON ROSEDALE: No worse than checking out an unknown pain a person has, or checking stool for blood to see about colon cancer. Waist to hip ratio is less invasive than taking blood. And it’s a great thing for everyone to do at home. And you can start to at least get a question mark in your head that maybe you need to do something to increase your health and longevity.