Ron Rosedale recommends adequate protein and warns that excess protein is bad for health.
He gave this talk at the American Society of Bariatric Physicians (ASBP) meeting Oct 31, 2006. They’re medical experts who work to reduce obesity. As part of the 2006 presentations, the ASBP included a special segment that featured low-carb diets, researchers and scientists who are connected to the Nutrition and Metabolism Society. Special thanks to Instatapes for recording this presentation.
Listen to Ron Rosedale speech (40 minutes)
View PDF of keynote presentation that includes citations.
The good, the bad, and the ugly of protein.
The good, and that’s pretty good, is that we can’t live without it. It is a required nutrient. It’s an essential nutrient. Unlike carbohydrates, which is a nonessential nutrient, which means you don’t have to have any. With carboydrates, you can make whatever you need. With amino acids, you have to take some of them in.
Then we could go into a lot of the miscellaneous problems with proteins. I’m not going to go into that a lot. A lot of articles will show detriments to protein, and as Mike Eades mentioned, there’s a lot of articles will show it’s not detrimental. So it’s confusing. Whenever it’s confusing, it means you’re not going into it deep enough. You’re not go-ing deep enough into the basic science of it all.
Dairy products aside, when past and present meat consumption is factored in, there’s a three times risk of developing Alzheimer’s in meat eaters as opposed to vegetarians. Is that true or not? I don’t know. I don’t place a lot of emphasis on this kind of study. I want to go deeper because there is a lot of confusion. Here’s another study: High protein diet may precipitate a progression of coronary artery disease. Through an increase in lipid deposition and through inflammatory and coagulation pathways. Now if this is true, there must be underlying causes of this. That’s really what you want to get into to determine the truth of something.
We know that high protein can raise glucose. And I’m sure Mike Eades showed you studies where a high protein diet reduced blood sugars and was better for diabetics. But the question is, compared to what. If you compare a diet to the average American diet. If you change anything in the average American diet you’re going to improve it. Improving the American diet is not a trick. It’s like a race between a one-legged man and a grandmother. Who cares who wins that?
Here we’ve seen, if you eat a high protein diet, we’re going to go deeper and deeper and deeper into the science of all this. To see if there’s something to really tell us whether excess protein is good or bad. If you eat a high protein diet, there is excess stimulation of the transport to the liver. You flood the liver with amino acids, and it’s got to do something with them. You can do two things with protein. You can make protein, you can replenish the parts that have been torn down, or you can burn it for fuel. Hopefully, you’re not going to excrete it. Food was too precious in our evolutionary his-tory to waste it. Certainly, if you have protein in your urine, something is wrong. Burn it, or use it.
Rapid stimulation of the liver glycine cleavage system in rats fed a high protein diet. In other wods, you’re going to break down a lot of it if you eat a lot of it.
Glycine metabolism is stimulated by high protein feeding.
Effect of high protein intake on Insulin secretion and glucose. Hepatic glucose was sig-nificantly increased with high protein intake. It makes sense. If you have a bunch of amino acids floating around, your liver breaks extra protein into glucose forming carbon shells.
Insulin mediated suppression of hepatic glucose production was impaired with high protein intake but not in patients with a normal protein intake. Gluconeogensis was increased with a high protein diet. We conclude that a normal protein diet is accompanied by delayed progression of the continuous loss of endogenous insulin. We know that in diabetics, there’s a loss of islet cell function over time, and here they’re saying that high protein may contribute to that.
After adaptation to a protein restricted diet, if you restrict protein, diabetics experienced a 30% decrease in daily glucose concentrations, and I know from my practice, and this wasn’t in everybody, but if I had a diabetic, and I put all of them on a low carbohydrate diet. It doesn’t make sense to feed diabetics sugar. But in those that had more trouble processing sugar, the next step was reducing their protein, and I’d restrict it a lot, for an average size adult, I’d put them down to 50 grams a day, maybe 30 grams a day, and their sugar would then go down. So this isn’t just theoretical.
We conclude that severe protein restriction decreases insulin requirements in Type 1 diabetics and fasting hepatic glucose output and basal insulin levels in normal people. Not just diabetics.
We know that protein increases levels of insulin. We know that there’s an insulingenic effect in eating high protein. That’s well known. There’s also a leptin increase with pro-tein. Amino acids increase leptin. Continual high levels of insulin and leptin cause insulin resistance and leptin resistance. So you might get a short term benefit from high protein, but it may be at a price of a long-term detriment, If you keep those levels high. If you raise insulin you’re going to lower sugar temporarily until you become more insulin resistant, and if you raise leptin, you’re going to be less hungry, temporarily, until your hypothalamus becomes more resistant to its action. Which is will become by overexposure. It’s like if you’re in a smelly room, after a while you can’t smell it, the longer you stay in there.
Your cells work the same way. If they’re over-stimulated, they just put in earplugs. They don’t want to be yelled at.
Central nervous system. There’s a more critical role for leptin than insulin in mammalian energy homeostasis. People are ignoring leptin, but it’s probably more important than insulin in diabetes. And in all of the energy storage diseases. Metabolic syndrome, aging.
Why isn’t this really being told? Because there are no drugs that control leptin. So drug reps aren’t telling you about this. But, It can easily be controlled through diet. It is what tells you how to eat. You eat to control insulin and leptin. It’s very simple. Certain eating behaviors extend lifespan. They’ve shown that with dietary restriction. They thought it was calorie restriction, but it’s not. It’s restricting certain elements in the diet. Sugar and protein. Not fat. That’s a critical thing to understand.
In obesity, results of several studies show that chronically elevated central leptin, decreases hypothalamic leptin receptor expression and impairs receptor protein levels and impairs leptin signaling. So chronically elevated leptin contributes to leptin resistance, and leptin resistance leads to further obesity, leading to a vicious cycle of escalating metabolic devastation.
You can find a vicious cycle in almost any chronic disease. That’s why your body can’t deal with it. The way it deals with it ends up worsening the problem.
Lower leptin concentrations appeared to occur without evidence of increased hunger. If you lower leptin you improve leptin sensitivity. It’s suggesting a functional improvement in the resistance to leptin. The way to fix leptin and therefore obesity and therefore aging and diabetes and all sorts of things is by chronically keeping leptin down, your hypo-thalamus can increase sensitivity to it and listen to it. Not just by trying to up it. When leptin was first discovered that’s what they tried to do. Just give more leptin. How have they been treating diabetes? Give more insulin. Just up and up and up the insulin. No! You have to down and down and down the insulin. And give the cells more room to listen.
Communication is more dependent on listening actually, than speaking. Cells have to be able to listen to the signal.
If I were to start screaming at you, how many people will stay in this room? You’d cover your ears.
Response to energy restriction involving leptin concentrations is affected by dietary composition, not drugs. Macro-nutrient composition of the diet affects leptin. This is just saying that different protein compositions, different macro-nutrient compositions affected leptin.
On the high protein diet, the leptin messenger RNA did not decline upon fasting after a meal. It stayed up for a while. Chronically elevated leptin causes leptin resistance and leads to metabolic devastation.
Regulation of leptin secretion from white adipocytes by insulin glycolated substrates and amino acids. So the two things that will cause leptin spikes and chronically elevated leptin are sugar through a pathway called the hexosamine pathway and amino acids.
Amino acid precursors of citric acid cycle intermediate potently stimulates basal leptin secretion, insulin having an additive effect.
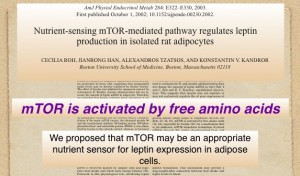
And the MTOR is one most people don’t know about yet, which is unfortunate. Because the MTOR pathway is intriguing, and may be one of the most, if not the most, important nutrient sensing pathway in the body, aside from insulin. And here, if you get nothing out of this talk, but this one sentence, MTOR is activated by free amino acids. MTOR is a pathway that senses protein concentrations. More specifically, amino acid concentrations. MTOR is also linked to leptin, and amino acids stimulates MTOR stimulates leptin.
Protein increases leptin, also triggers the hexosamine pathway, and the ugly. High protein apparently accelerates aging and therefore all the chronic diseases associated with aging.
The role of specific nutrients in caloric restriction. Dietary restriction has been shown to increase longevity which indicates it’s having positive results. However, it appears it is not caloric restriction but the carbohydrate and protein restrictions in the diet, the medi-ate the effects, at least in flies, and it appears in other organisms, also.
Why would protein be so important in the regulation of aging. Life is a constant battle between damage and damage control. If we could repair damage as fast as it occurs, we would live forever. Ultimately, unfortunately, we damage the damage control mechanisms, and that’s really what does us in.
Excess protein actually increases damage and reduces our ability to repair it, so it’s a double whammy.
Life at higher temperatures leads to a greater accumulation of irreversible damage that leads to death. One of the advantages you’ll hear all over the place is that it’s good to be thermogentic. If you go to a health food store, there are thermogenic aids all over the place. And one of the advantages given to a high protein diet is that it’s thermogenic. And it is. Without question, protein is the most thermogenic nutrient you can eat. It will produce the most heat. Well producing heat and living a long life are just not compatible.
If you went to a gas station and there were two pumps, and one said this pump will produce the most fuel efficiency and give you the most mileage, and this other pump will cause your car to run hotter . . .
Which one are you going to get? You’d never get the one that makes your car run hotter because what’s that going to do to your engine. Not good things. That’s why you have a radiator.
Protein increases glycation, oxidation damage, and we know that protein increases growth hormone and IGF-1. In the last talk, I constantly hammered that high IGF-1, and insulin promotes aging, through a separate pathway. We know that protein increases IGF 1 and AGES, the short term for Advanced glycated end products. There are two major causes of aging. One is oxidative damage and the other is advanced glycated end products, that’s when glucose combines with proteins and DNA. Basically glucose is a sticky molecule that changes the shape and function of whatever it sticks to. It forms what are called advanced glycated end products, the acronym being AGES and that was intentional because it plays such a major role in the chemistry of aging.
In some cells AGES increase with amino acids. In another study, profibrotic injury response occurred in messengial cells exposed to amino acids with or without high glucose by formation of AGES, oxidative stress and activation of the protein kinase Beta and Map Kinase pathways. Which are cell proliferation pathways. Calorie restriction slowing aging and extending life. Mice with pituitary glands devoid of growth hormone producing cells exhibit a remarkably extended lifespan, as do genetically altered mice where they targeted the disruption of the growth hormone receptor, which results in low concentrations of IGF. Andre Barke has done a lot of work on this. Wonderful man, and he’s now head of the American Aging Associaton. And he’s shown convincingly that when you keep insulin and IGF down, animals live a lot longer. And he recently won the Methuselah prize for the longest lived mouse.
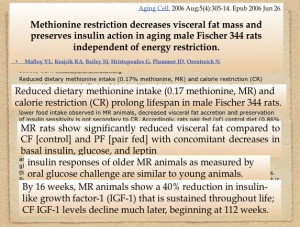
Reducing protein extends life. If you restrict methionine, you decrease visceral fat mass and you preserve insulin action. Reduced dietary methionine and caloric restriction pro-long lifespan. In other words, it isn’t just caloric restriction. If you reduce dietary methionine without caloric restriction, you get the same thing, Methionine restricted rats shows reduced visceral fats, with decreases in insulin, glucose and leptin. Insulin responses in older methionine-restricted animals as measured by oral glucose challenge are similar to young animals. By 16 weeks, methionine restricted animals show a 40% reduction in IGF, which is sustained throughout life.
For 60 years, the only dietary manipulation showed to retard aging was Calorie restriction, and more recently, they’ve shown that it isn’t necessarily calories. If you decrease tryptophan, and you decrease cystine and methionine, you get the same thing. Methionine restriction is not a consequence of reduced energy intake. The intervention alters the rate of aging and not by correcting a single defect.
Recent work has shown that dietary restriction in fruit flies is a product of acute effect on genetic transcription that causes fully fed flies to adopt the mortality profile of lifelong dietary restricted flies within 40 hours of initiation. In other words, you don’t have to do this starting from an infant. If you adopted some of these today, you can get the same genetically healthy profile, the same healthy genetic transcription profile, as if you had been dietary restricted all your life.
In other words, you can do this at any time. You can experience the benefits of this. You can go back in time, essentially.
You can reduce your aging to a certain extent and therefore the diseases associated with aging, if you just adopt this now.
Alterations in nutrient related signaling pathways are thought to initiate the cascade of changes that underlie longevity assurance by dietary alterations.
The nutrient sensing pathways, that’s what is critical.
Insulin and IGF alter lifespan in rodents and many other species. Insulin is known to be involved in regulation of homeostasis in response to a diet, and is know to be a link between the calorie of the diet and extended action. However, two lines of evidence indicate that insulin and IGF are not the only pathway. If you reduce insulin IGF activity and then put them on a dietary restricted program, you have an added effect. They seem to function by two separate, parallel pathways. Reducing insulin and IGF are definitely good. You go further and what’s that pathway? MTOR. It’s a parallel pathway that operates alongside the insulin pathway, but apparently, separately.
These studies provide further support to the argument that protective effects of dietary restriction are not limited to calories alone but involve an aspect of protein metabolism as well. Sugar and protein. That’s what was available when all these signals arose, evolutionarily.
Lifespan is important not because Nature cares about you, but it cares about reproduction, and it wants you to reproduce at a future, more opportune time, if the nutrient availability isn’t good now. But we can use that knowledge. We can still dig into pathways that affect aging and health by what we eat.
A little more on MTOR. The amino-sensitive MTOR pathway from yeast to animals. The target of rapamycin, which is a drug being investigated for cancer, and heart disease and autoimmune diseases and many things. It’s a natural substance discovered by accident. They didn’t know how it worked, but that’s how MTOR pathway was found. Maybe less than 10 years ago. They found it was extremely important, and we’re going to understand that any effect of rapamycin is paralleled by low amino acids. Rapamycin inhibits MTOR. That’s what it does. That’s how it works. How it works to reduce cancer.
In a 2002 study, they reported that the process through which nutrients, amino acids, activate MTOR are largely unknown. They said then that evidence exists for both an intracellular and membrane bound sensor for the amino acid. Since then, they have a clearer idea of how it works.
Studies performed in fat cells, in ovarian cells, in liver cells, in muscles, pancreatic beta cells all show a sensitivity of phosphorylation status of MTOR subtrates and amino acid concentrations. In other words, it appears to work everywhere. All cells have apparently an MTOR signaling pathway that is sensitive to amino acid concentrations.
Indeed, activity of MTOR was determined by amino acid availability in each cell line tested. That is the main thing that will stimulate MTOR. It is an amino acid sensing pathway.
Here’s an interesting comment: Future studies that examine the link between amino acid transports and MTOR activity will resolve the initial signaling events that result in the activation of MTOR targets and will provide insights into the scavenging of nutrients by malignant cells. Malignant cells try to hoard amino acids, and when they do so, they upregulate MTOR, and when they up-regulate MTOR, they stimulate cell division.
Here we show that inhibition of MTOR activates apoptosis. One of the ways that cancer is allowed to progress by shutting off P53. P53 is one of the ways that we kill cancer. It’s a checkpoint. P53 triggers cell suicide, which is known as apoptosis. Course, cancer cells don’t want that. So they mutate, or inIn some way, P53 got mutated, and it can’t trigger that cell suicide. And here, it’s showing that rapamycin, by down-regulating MTOR, can trigger cell suicide without P53. It’s another checkpoint. In other words, keep amino acids low, and you can check that cancer in its tracks.
The TOR pathway regulates genetic expression by linking nutrient sensing to histone acetylation, and the promise of rapamycin as a cancer drug is being explored. This is in 2003. It’s been showing remarkable antitumor activity in cells. We therefore find it intriguing that rapomycin results in a gene profile seen in amino acid limitation.
There are two things seen in cancer cells require to keep going.
Two things any cell requires. Fuel and parts, the main parts being protein. It’s a requirement for cancer. It doesn’t take a lot of intelligence to know that if you want to suppress it, just don’t eat it.
Don’t give it sugar. Sugar can be used as an anaerobic fuel. You can burn sugar without oxygen. You have to have oxygen to burn fat. Cancer cells are rapidly dividing, and they mostly will outplace the supply of oxygen. The most aggressive cancer has to use sugar as a fuel source. One way to suppress cancer is just not to feed it sugar. But this isn’t some elegant drug, or some profit induced therapy, so it’s not being used. I’ve seen remarkable results by just eliminating sugar form the diet. And that means potatoes, pasta, rice and all that stuff that turns into sugar immediately. Another way is by toning down the amino acids. Now you have to have some. But we know that if you restrict amino acids, your body goes into an amino acid conservation mode.
Extension of chronological lifespan in yeast by decreased TOR signaling. TOR signaling regulates multiple cellular processes in response to nutrients, especially amino acids, raising the possibility that decreased TOR signaling mediates extended lifespan in caloric restriction. In support of this possibility, removal of either aspartame or glutamine from the media feeding the yeast significantly increased survival. Pharmacological Inhibition of TOR by rapomycin also increased lifespan.
We propose an up-regulation of a highly conserved response to starvation-induced stress is important lifespan extension by decreased TOR signaling in yeast and higher eukaryotes. Us.
There’s distinct signaling down stream. A lot of research going into MTOR. Key roles in regulating cell and animal growth. The cell cycle, gene expression. Recent studies have shown that MTOR is essential for cell growth and proliferation Rapamycin as a specific inhibitor of MTOR is in clinical use or potential use in graft rejection, restonosis after angioplasty, cancer angiogenesis, liver fibrosis and many other diseases. There is general agreement that amino acids do indeed stimulate the phosphorylation of MTOR downstream targets. Amino acid infusion during a euglycemic hyperinsulemic clamp in fasted humans decreased rather than increased glucose disposal. Raising glucose. Although these data may be explained by substrate competition. Ie, the Amino acids were oxidized instead of glucose. Which it is. Certainly partially. But there are indications the amino acids cause a time dependent rapamycin sensitive down regulation of protein kinase B and of glucose transport by insulin. In other words, it causes insulin resistance.
Another example suggesting that amino acids may cause insulin resistance is that of glutamine. This amino acid, which is a potent stimulator of glycogen synthesis is also a substrate for the hexose monophosphate shunt, and has been shown to highly regulate insulin sensitivity.
The importance of amino acid signaling in the coordination of whole body metabolism is also indicated by its involvement in the regulation of leptin production by adipocytes. Amino acids upregulate MTOR. Cause spikes in leptin.
There is an amino acid dependent signaling that controls lepin production via adipocytes.
The MTOR signaling pathway is frequently over-activated during cancer. Thus, the importance of amino acid signaling in cancer is evident.
When we’re talking about life extension in animals, we’re generally talking about reduction of cancer. Most laboratory animals die of cancer or autoimmune disease, so if you extend lifespan in laboratory animals, it’s synonymous with reducing cancer.
Another way that lifespan appears to be enhanced is by regulating protein turnover. You have to get rid of rotten proteins. We talked about AGES, and how glucose sticks to proteins and cause Proteins become malformed and do nasty things, so we have to get rid of them. Tear them down. We know with caloric restriction and other methods that enhance lifespan, you accelerate the breakdown of old proteins and manufacture of new proteins.
Proteozome mediated proteolysis and autophagic proteolysis declined with age. However, the last two pathways can be considered an anti-aging repair mechanism because they remove aberrant proteins and defective cellular organelles.
Caloric restriction not only increases proteozome proteolysis. But also autophagic proteolysis, which may contribute to increased longevity. When you upregulate MTOR you down regulate proteolysis.
The best drug to reduce MTOR signaling, to slow aging and the chronic diseases associated with it is already available. Avoid high protein.
But what is that? What is high protein. You can go to a lot of textbooks that talk about .6 grams per kilogram. But one study that I think is very interesting . . . You can get into a ballpark. When you talk about 2 to 3 grams of protein per kilogram of lean body mass, that is certainly too much protein.
But what is the requirement in an infant, infant, being breastfed. Young infants, 2 months old, have the highest protein need. They’re growing rapidly. Brain is growing. The protein content in breastmilk is about 1 gram per 100 milliliters, and the daily intake is approximately on 1 gram per kilogram per day. That’s what nature says is the requirement of a growing, breast-feeding infant.
When other foods are introduced during the weaning period the protein intake Increases remarkably to 3 or 4 grams of protein per kilogram per day in spite of the fact that the protein requirements are decreasing. The long-term consequences are obscure. Although I think the MTOR signaling are telling us what those long-term consequences might be. A high protein intake has endocrine effects such as it increases insulin, increases IGF, and we know these hormones increase the rate of aging. Furthermore the metabolic effect of high urea and many amino acids may exceed the kidney and hepatic system’s ability to metabolize and excrete the excess nitrogen.
In other words, when you use protein as a fuel, you take off the excess nitrogen, and then you have to do something with it. Because, it’s a poison. If you take too much, It causes acidosis in the blood and that causes redistribution of calcium and magnesium, and all sorts of things, and what the consequence are for that is manifold.
So what’s high. Certainly above 1 gram per kilogram of lean mass is probably high.
Most people, I’ll put on .7 or .75 grams per kilogram of lean body mass.
But if I’ve got a diabetic, and I really want to reverse their aging, which means reverse their diabetes, because diabetis is a model of aging, I’ll put them down to .5 or .6 grams per kilogram of lean body mass per day.
So what’s left to eat?
We know that sugar, foods that turn into sugar, raise insulin, IGF accelerate aging, worsens diabetes. It’s horrible for you. Now I’m telling you that extra protein isn’t good for you either. It appears to accelerate the MTOR pathway and has all kinds of debilitating effect, not the least of which is stimulating cancer.
Fat. Eat fat.
Fat appears not to stimulate insulin. It does not stimulate the MTOR pathway. It does not cause an increase of leptin and in fact it keeps it down. And our health is going to be dependent on what our hormones tell our brains to do, whether to be hungry or not. If you keep leptin down and your hypothalamus can listen to leptin, you are not going to overeat. When leptin is down it stimulates fat burning. It helps diabetes. It helps all sorts of things. I’ve been doing this for over two decades now, and I can tell you for sure it happens.
You have to regulate the hormones that regulate your brain, and you do this by diet, and then you can affect the rate of aging and the incidence of the diseases associated with aging.
Special thanks to Greg and April at Instatapes for helping to track down the audio of this talk, and to Ron for permission to post the audio, transcript and PDF of the citations used in the talk.





20 comments for “Ron Rosedale – Protein: The Good, The Bad and The Ugly”