 Ron Rosedale challenges the new Harvard Study, published this week in the Journal of the American Medical Association. He says the study itself has many good points regarding the importance of noting that not all calories are equal, and reducing carbs may be more important than reducing fat. But in press reports, he’s concerned that the “winning” diet that the Harvard group prefers does not deserve the crown . . .
Ron Rosedale challenges the new Harvard Study, published this week in the Journal of the American Medical Association. He says the study itself has many good points regarding the importance of noting that not all calories are equal, and reducing carbs may be more important than reducing fat. But in press reports, he’s concerned that the “winning” diet that the Harvard group prefers does not deserve the crown . . .
I’m Shelley Schlender, for Me and My diabetes. U-S nutrition policies are based on ” calories in, calories out,” meaning count your calories and burn off any excess with exercise. Late in June, 2012, the Journal of the American Medical Association raised a challenge to that idea by publishing a Harvard study involving three different diets, and how each diet affects the likelihood of gaining weight. The diets being studied were a low-fat diet, a low carbohydrate diet, and a diet with some protein, and then equal amounts of calories from carbohydrates and fats – the so-called Mediterranean diet. The research group measured health markers such as blood triglycerides, metabolic rate, blood sugars, hormones such as insulin, leptin and cortisol, and inflammation markers that included C-Reactive protein. It was a studied that challenged current policies about “calorie in-calorie out” because changes to the health markers were strongly influenced by just which diet the test subjects ate. In many ways, it’s a first-rate study. But then, the study was interpreted in the media in a number of wildly varying ways, and much of that interpretation was influenced by just who got interviewed for the reports. David Ludwig, one of the study’s leaders, was a prominent voice in the media reports, and Ludwig told many media outlets that while the low-carb diet had the MOST improvement in health markers overall, the fact that it raised cortisol levels and didn’t lower C-Reactive protein as much as the Mediterranean diet did, means the Mediterranean diet is the best one. Now, the Harvard School of Nutrition has been a long-time advocate of Mediterranean Diets. So to check out their conclusion from someone who is NOT an major advocate for Mediterranean Diets, up next, we talk with an advocate for Low-Carb, High Fat diets, Dr. Ron Rosedale. (Transcript Follows)
Calories In/Calories Out VS. Hormones Signaling
Ron Rosedale, do you believe current dietary policy that stresses a calorie in is a calorie out, that what we need to focus on is how many calories we take in and then exercise enough that we don’t end up with excess calories?
RON ROSEDALE: Well, I guess that’s been the dogma for decades. I suppose if it had been correct, you wouldn’t see not only the maintenance but the ever-increasing incidence of obesity and diabetes that’s occurring worldwide as that supposed dogma has been followed. What I think the literature shows and has shown for at least a couple of decades, but the scientific evidence for this is just being ignored continually, is that the story is a bit more complex than that, and that whether we burn fat or not, which is what will determine whether we’re obese or not and whether we in most cases contract diabetes or not, is controlled by very specific hormones that regulate metabolism, the main ones being insulin and, even more importantly, leptin. It’s those hormones that are in turn controlled by what we eat.
And it isn’t just the levels of a hormone that are relevant, but much more relevant, in fact, the only relevance, is their activity. The activity is determined not just by the level of the hormone, but more importantly, by the cell’s ability to listen to that hormone. An example is the well-known phenomenon of insulin resistance, which occurs in the vast majority of cases of diabetes and essentially is the sine qua non of so-called type 2 diabetes, which is better called insulin-resistant diabetes, where the person has plenty of insulin but the cells aren’t able to listen to it and therefore they behave as if the insulin level is too low and then ultimately blood sugar goes up, but the consequences are much deeper than that. The disease is not from too little insulin, it’s not from too weak a signal, it’s from an inability to listen to that signal. And the inability to listen to that signal is most likely caused from an overactivity of that communication over time.
It’s too much, so the cells tune out?
RON ROSEDALE: Exactly. It’s kind of like being overexposed to noise. You lose your hearing faster. Or sitting in a smelly room for a long time, pretty soon you can’t smell it. The stimulus becomes too much, as you mentioned, and the chemical mediators of that signaling basically become depleted, and the pathway becomes resistant to the signal. And that resistance is paramount to virtually all of the chronic diseases of aging, and perhaps even aging itself. The same thing happens with leptin, where obese people have plenty of leptin that normally signals that you have too much fat and you’d better burn it off, and you curtail your hunger so you don’t eat as much. But the actual event that occurs with leptin resistance is the opposite, where although leptin should be telling the brain that you have too much fat, the brain is hearing that you have too little and that you won’t be able to survive a famine and that therefore you should be hungry and you should store more fat and you should not burn the fat that you’ve got.
That’s really the ultimate basis of almost all cases of obesity around the world. It goes even beyond that, because then there are inflammatory markers, and many people believe that the same processes control the actual rate of aging. These are all tied into a genetic pathway that we know controls the rate of aging in many species of laboratory animals, as indicated by calorie restriction studies. It goes on and on and on.
So the simple adage that a calorie in is a calorie out is really, really archaic and really needs to be thrown out.
The Harvard Study
There’s a new study out of Harvard where the headlines about it today are that a calorie is not a calorie. There’s a different process that’s governing whether or not what we eat is helping us lose weight or whether what we eat is helping us maintain our weight, which may be even a bigger deal, because there are a lot of ways that people can lose weight, and in the U.S. and in modern countries, it seems the biggest problem is keeping that weight off. This study compared three different diets, a low-carbohydrate diet, a high-carbohydrate, low-fat diet, and then Mediterranean diet where supposedly there wasn’t anything quick-to-absorb starch or sugar that caused blood sugars to spike, there were a lot of complex carbohydrates, and there was a moderate, not low, amount of fat. The researchers compared these diets and got different results. What do you think of the idea of doing that kind of study?
RON ROSEDALE: First I want to say that what really surprised me about the study is that it’s news. It’s been shown for a couple of decades by myself and many others that a calorie is not a calorie. They’re certainly far from the first people who have shown anything like this.
As far as the study is concerned, I hate to say it, but as in so many medical and nutritional studies, it really is designed to try and support a preconceived conclusion. The Harvard/Boston researchers wanted to try to support a dietary protocol that they’ve been using for many years, which is the so-called Mediterranean diet.
Let’s give a bit more detail about the study. It was published today in the Journal of the American Medical Association, this is June 27th, 2012. The title of the study is “Effects of Dietary Composition on Energy Expenditure During Weight Loss and Maintenance.” One of the authors is David Ludwig. The lead author is Cara Ebbeling, who I hope to speak with. As you say, this is a group that overall has been strong advocates of the Mediterranean diet . You’re saying, though, that in the study and in their media reports about it, they stacked the deck in favor of the Mediterranean diet?
RON ROSEDALE: They tried to stack the deck, but the results actually didn’t support their conclusions. It kind of surprised me that they concluded what they concluded, that the Mediterranean diet was the best diet. What their research really showed, and what they even said in the research paper, was shown, was that the very low carbohydrate diets actually had the best results as far as metabolic markers, with what they said were two exceptions.
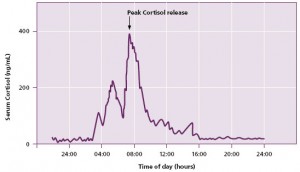
Cortisol – Total Daily Level VERSUS Diurnal Pattern Throughout the Day
RON ROSEDALE: One of the major exceptions that they mentioned, which they said was an adverse result, was that cortisol levels were increased with the very low-carbohydrate diet. And that’s probably true.
It’s true that cortisol levels were increased, or that it was an adverse effect?
RON ROSEDALE: It’s true that cortisol levels were probably increased and would probably increase with a properly administered very low-carbohydrate diet. What was wrong with the conclusion is that it’s an adverse effect. It’s actually a very beneficial effect. You will see with calorie-restricted studies in animals that it has been shown to extend lifespan for the last 80 years and what’s seen in centenarians, people who live to be over 100, in all of these groups, one of the common findings is that cortisol levels increase. The study was saying that this is a bad thing, implying that an increased cortisol level shows that there must be increased inflammation.
But one of the reasons that cortisol levels increase as theorized is to suppress inflammation. Cortisol itself is a very powerful anti-inflammatory.
Are you saying, then, that depending on the composition of a diet, some of these hormones have different effects? That in a diet that high in carbohydrates and more than enough calories, extensive time with high cortisol might be more of a problem than it is with a high-fat, low-carbohydrate diet where people are not eating too many calories?
RON ROSEDALE: If you just measure hormone levels, and this is kind of what I was getting at at the beginning of the conversation, it doesn’t give you the full story. The fact, for instance, going back to diabetes and insulin, where insulin is elevated and yet the signal is very low, causing higher blood sugars, and the actual frank definition of diabetes, because of a low signal. So the fact that cortisol levels go up does not necessarily mean that the signal is up. You have to look at why it’s going up. Is it going up because it has to go up, because there is an overabundance of inflammation, or is it going up as one of the protective mechanisms to reduce inflammation long-term, as seen in calorie-restricted long-lived animals and centenarians?
Leptin went down the most on Low Carb
RON ROSEDALE: It’s even theorized that one of the reasons calorie restriction works to extend lifespan and greatly improve health is because reducing calories reduces inflammation. For instance, one of the major markers shown to go down in the Harvard study, was leptin. Leptin went down the most on a very low carbohydrate diet. That’s extremely significant, because we know that leptin controls many inflammatory markers. And again, one of the numerous papers now that have theorized that one of the reasons behind the health benefits and longevity behind caloric restriction is a lowering of leptin, which controls the neuroendocrine access via the hypothalamus in the brain, which then controls every other hormone in the body and also controls inflammation and by going down, greatly suppresses many different markers of inflammation. As part of a long-term maintenance to improve lifespan, it reduces inflammation and also by reducing blood sugar, which lowering leptin can do irrespective of insulin, improving insulin sensitivity and leptin sensitivity also greatly reduces the cause of inflammation and not just the mediators of it, since we know that glucose itself is highly inflammatory, as is insulin and as is leptin.
So what the study really showed is that if you go much further than their Mediterranean diet and you reduce carbs by not just slowly absorbable carbs, but just reduce them altogether, because even the slowly absorbable carbohydrates will cause a spike in carbohydrates, will cause a spike in blood sugar, just not as severe as some other carbohydrates.
Am I correct in saying that you think that just looking at one hormone without looking at the whole symphony doesn’t give you the entire picture? You seem to be saying that, for instance, in somebody who was a diabetic, who had insulin resistance, who was obese and had high blood pressure, if that person’s cortisol levels were high, that might not be the same as when someone who is thin and fit and caloric restricted or has the markers of the centenarians, the people who live to be in their hundreds and are healthy, or the people who are on a restricted calorie diet, that’s a different kind of high cortisol for them than it is for somebody who is a type 2 diabetic or somebody who’s a post-traumatic stress victim.
CORTISOL – Was it High in the Morning and Low at Night?
RON ROSEDALE: That’s absolutely true beyond the obvious. The reasons behind an elevation in a hormone are extremely important, but also what is mediating the elevation and when. For instance, in this study, in which they’re trying to hang their hat on cortisol as the reason that their Mediterranean diet might still be better than a very low-carbohydrate diet, even though the very low-carbohydrate diet showed an improvement in all other metabolic markers, what’s relevant on cortisol is that we know that it is normally secreted in a diurnal pattern, meaning that typically if you’re healthy, it ought to be released in high quantities in the morning and low quantities at night.
This would have had to have been measured. Many, many studies now have shown that a disruption in that diurnal secretion of cortisol is what can cause many of the problems in cortisone, not the absolutely amount, but when it’s released. That’s extremely important. So what’s found in centenarians, for instance, is that the diurnal variation in cortisol is maintained, so even though the cortisol levels are increased in centenarians, the good part is that they’re increased appropriately. They go up in the morning and down at night, and that diurnal variation in many disease states becomes decreased.
You’re saying that a bigger clue of whether or not cortisol is healthy isn’t the amount, but whether it is being released in an appropriate way from morning through night?
RON ROSEDALE: Right. And in this study they didn’t measure that. They measured urinary 24-hour secretion, which doesn’t—you can’t just measure the total amount of cortisol. They didn’t measure cortisol binding protein, I don’t believe. So it’s not just the amount of cortisol but when it’s released in any of the fatty especially steroid molecules, such as HDL and LDL and testosterone and all the steroids that are derived from cholesterol, which by the way is a precursor for all the steroid hormones, including cortisol and testosterone and estrogen. Cholesterol is not that evil monster that the medical profession is making it out to be, but in fact is a life-giving molecule.
But the metabolites from cholesterol are all kind of a steroid waxy, fatty substance and have to be carried around the bloodstream. They’re carried by binding proteins to make them soluble in the watery environment of the blood. So LDL is low-density lipoprotein and HDL is high-density lipoprotein. These shuttle cholesterol to and from tissues. You have the same type of molecules that shuttle cortisol and shuttle testosterone and shuttle estrogen. For cortisol, they’re called cortisol-binding proteins, and the proportion that is bound to a protein is inactive. It’s only the free fraction that is active. So if you just measure cortisol levels, you don’t know the amount that’s active and the amount that’s inactive. And if you just measure 24-hour secretion, you don’t know when it’s secreted and when it’s not secreted.
In other words, it gives you almost no information. So trying to hang your hat on the fact that cortisol levels were elevated and saying that therefore, their Mediterranean diet is better than a very low-carbohydrate diet is extremely misguided.
Is there a way to measure the kind of cortisol that is in the active form? Did they measure that?
RON ROSEDALE: Oh, yeah, there’s definitely a way to measure it, and no, they didn’t measure it. You can measure it directly in the blood, or more appropriately, you can measure it in the saliva, which in most cases is an easier way to measure it because then you can easily collect it both in the morning and the evening, so that you can at least get two measurements, and the salivary measurements of cortisol are free fractions, the amount of cortisol that actually got into the saliva, that actually had activity.
And then again, you have to go beyond that, go beyond the assumption that cortisol is bad. It’s not. You need cortisol. Again, it’s an anti-inflammatory. It’s not a pro-inflammatory.
Are you somebody who would give someone a cortisol shot if their hip or their knee was sore?
RON ROSEDALE: No, I wouldn’t. You don’t want it in super-physiologic doses, typically.
So there are ways that you think that it’s good and ways you think that it’s bad. But when it appears in the blood or the saliva in higher amounts in the right pattern during the day and the night, that generally tends to be an indicator of health, not disease?
RON ROSEDALE: Exactly. Like any hormone. Insulin is not a bad thing, it’s a good thing. Leptin is not bad, it keeps you alive. You have to get the signal’s message across to the cells. That’s really what you want. You want to cells to listen appropriately, at the appropriate time and at the appropriate location. That’s what is necessary for any type of health.
I wondered also with cortisol, in the case of somebody on a very low-carbohydrate diet who’s eating a lot of fat, which a third of the people in this Harvard study were doing, whether that would affect cortisol levels. You see, when someone’s not eating many carbs, the body has to send out signals for the body to make its own sugar now and then, just to keep the levels regulated. One way to do that is for the body to send out a cortisol signal, is my guess. Is that correct?
RON ROSEDALE: That’s correct. One of the purposes of cortisol is as a gluco-regulatory hormone. If sugar levels go low, then cortisol is one of the hormones that will be secreted so that you can raise glucose to a level that the body deems appropriate. The real key is to get that level as low as possible.
But when the body gets to call the shots on maintaining the blood sugar level with something like cortisol, it gets to choose what that level will be?
RON ROSEDALE: It gets to choose, and over time, and this is another key, the level becomes lower. In the Harvard Study, they didn’t allow enough time for research subjects to adapt to the low carb diet in order to show this effect..
You mean that the level of cortisol over time is likely to go down further if somebody gets even more adapted to a low-carbohydrate, higher-fat diet?
RON ROSEDALE: Yeah. They only carried out the experimental diets for four weeks. That’s just about enough time to get a person adapted, and not longer. They were measuring cortisol at a time when their tests subjects were not really adapted yet to a very low-carbohydrate diet. You need to partake in that metabolic change much longer, and the set point then for glucose goes down, and therefore the need for gluconeogenesis goes down. But more importantly, there is a metabolic adaptation that will increase the ability to manufacture glucose from other metabolic precursors such as lactates and glycerol in the body, such that the need for the major gluconeogenic pathways is greatly reduced. But that takes quite a few more weeks than they carried the study out.
Your comments makes it sound as though it would be helpful to ask the Harvard Researchers whether the cortisol levels in people on a low-carb, high-fat diet went down more at the end of the four-week period when they were eating low-carb, than at the beginning.
RON ROSEDALE: That would be, and I didn’t really see how many times the Harvard researchers actually measured cortisol. I don’t know if it was a before-and-after or if there were any intervening measurements. But again, you don’t know necessarily whether it’s a good or a bad thing. As I mentioned, cortisol is increased in all of the parameters that we know that increase health and lifespan in calorie restriction and in centenarians. And I think one can’t ignore that there might be some sort of benefit, then, to increased cortisol. My guess is that that would definitely be true, and my guess is that it is likely due to its anti-inflammatory effect.
Ron Rosedale Likes a Low Carb, High Fat, Adequate Protein Diet
Ron Rosedale, you have been suggesting that the Harvard Boston Hospital study stacked the deck in favor of the Mediterranean diet, and the way that cortisol was measured didn’t reveal some key elements of why an elevated cortisol level might not be an issue. You’ve said that the Harvard researchers have a vested interest in recommending a Mediterranean style diet. It’s fair to say that you’re someone who likes to stack the cards in favor of a high-fat, low-carb diet.
RON ROSEDALE: That’s because I’ve found that to be by far a better diet. I’ve used the Mediterranean diet in the past and didn’t get anywhere close to the results one can get if you just get rid of sugar. There is no biological necessity to eat sugar, and we know all sorts of adverse consequences, secondary to glycation, advanced glycated end products. We know that it increases inflammation in aging, it increases spikes in insulin and leptin, which promote insulin and leptin resistance, and if you increase glucose levels, whether it be by fast-acting glucose or by longer-acting glucose, the so-called resistant starches that they’ve maintained is beneficial on their Mediterranean diet, you accelerate aging. And in fact, we know through Cynthia Kenyon’s study and others, and what I’ve shown in studies, that if you keep glucose levels very low, and only if you keep glucose intake very low, only if you follow a very low-carbohydrate, not a high-protein diet, and a high beneficial fat diet, you can mimic the effects of calorie restriction as far as the laboratory parameters. And that can only be a good thing.
Harvard Study Used HIGH Protein in Low-Carb Branch
RON ROSEDALE: I also want to mention one thing on this study, that it is quite notable that they put people on a high-protein diet.
The characterization of this diet was that it was an Atkins-style diet that was high in fat and low on carbs. Are you saying that that was actually a high-protein diet?
RON ROSEDALE: They were putting people on an average of 150 grams of protein a day. That’s two to three times the protein that I recommend for people. And elevated protein has a lot of adverse consequences as far as many different parameters, including inflammation, which could be one of the reasons that they noted an increase, but a non-significant, I should mention, increase in CRP, which is their second so-called adverse effect that they encountered. C-reactive protein is a so-called marker of inflammation, but it’s really a marker of the immune system increasing. It’s like one of the first responders to increase the phagocytic activity, the ability of white blood cells to engulf intruders and clean up debris.
So once again, it’s certainly possible that short-term CRP could go up on a very low-carbohydrate diet secondary to the anti-aging effect, actually slowing the aging. One of the events that take place in calorie restriction and in other genetic modalities that greatly increase health and lifespan in laboratory animals is that you increase something called autophagy, which is the ability of the body to basically clean up garbage. That requires a more active immune system. It’s possible in a short term that you can increase immune activity to increase autophagy so you can get rid of some of the garbage that is poisonous to the body.
But I should mention that long-term, what I’ve seen in people on a very low-carbohydrate diet and what’s seen in calorie restriction is a reduced CRP longer term. After the initial several-week adaptation, I think you’ll see CRP come down. But it also should be noted that what their data showed and many other data showed, including myself, is what will lower leptin the most is a very low-carbohydrate diet, and when you lower leptin, you greatly reduce many different markers of inflammation, including, interleukins, many markers of inflammation. Leptin itself is an inflammatory chemicals. It’s a cytokine.
So other markers, had they been measured, they would have found secondary to lowering leptin, would have been greatly reduced, other markers of inflammation.
So one concern that you have here is, these are markers where in the short term, they can go up for beneficial reasons, and after a person is adapted to a high-fat, low-carb diet, they both tend to go down for again benign, helpful reasons. Another question to ask the researchers would be, did the C-reactive protein levels for the people on the high-fat, low-carb diet tend to start out higher and end up lower after four weeks?
RON ROSEDALE: Two things. Number one, what they are calling two inflammatory markers, cortisol is not an inflammatory marker. It’s an anti-inflammatory marker. They are misinterpreting cortisol.
You believe that cortisol depends on a lot of other things besides just that number alone?
RON ROSEDALE: Yeah. And again, cortisol, we know, and it’s being used therapeutically as an anti-inflammatory. It’s not pro-inflammatory, as they’re making it out to be, like an adverse event. It’s not an adverse event. I think they were trying to find some reason to downplay the beneficial laboratory results that were obtained with the very low-carbohydrate diet, even though they style of low-carb diet used much more protein than I would have recommended. Had they used a diet that I recommended, which would have been a much more moderated protein intake, probably a higher beneficial fat intake, and a very low-carbohydrate intake, you would get even far greater beneficial results. I’ve written much about it, and I think you can find on the Internet many adverse consequences of high-protein.
And when they mentioned an Atkins-type diet, that is true. An Atkins-type diet is basically very low carbohydrate and anything else goes. I maintain very strongly that that is not so. It’s not anything else goes. There’s a huge difference between a very low-carbohydrate, high-protein diet and a very low-carbohydrate, low-to-moderate protein diet. There are huge differences in longevity and other metabolic parameters on different metabolic pathways.
The current experts on the Atkins diet, who have written the New Atkins for a New You, are Eric Westman, Jeff Volek, and Steve Phinney. In their current writings about it, and in conversations with them, they would agree with you that you don’t want to have high protein as part of a low-carb diet.
Yeah. They agree with me because I taught them that. They were actually very pro-protein up until a meeting where I spoke at the American College of Bariatric Physicians quite a few years ago that kind of pitted me against everybody else who then was recommending a high protein intake. I showed them quite a bit of literature that high protein was not beneficial. I’m quite happy to hear that they’ve changed their tune since then.
If all of you “low carb” guys are saying that high-protein should not be part of a low-carb diet, then why did the Boston Harvard team use a high-protein diet as their high-fat, low-carb diet?
RON ROSEDALE: That’s a great question. Again, I think there are so many studies in health and medicine where the experiment is not particularly performed to find some ultimate truths but is performed as a marketing effort. I think they were trying to bolster their recommendation for a higher-carbohydrate, Mediterranean-type diet by the setup of the experiment to begin with, but also then in their conclusion, the data that was forthcoming from their study didn’t support their conclusions. And yet they tried to make it seem, and they popularized through their PR department and all the popular media, that their Mediterranean diet was far healthier than a very low-carbohydrate diet. That is not what their data showed at all.
 C-Reactive Protein Differences were NOT significant in Harvard Study
C-Reactive Protein Differences were NOT significant in Harvard Study
RON ROSEDALE: Again, on the cortisol levels, the high cortisol is almost synonymous with longevity and health in centenarians and calorie-restricted animals, which are two of the major modalities of aging studies. And the other so-called adverse effect that they’re reporting was C-reactive protein. And they have to emphasize and I have to emphasize that the difference in C-reactive protein between the very low-carbohydrate diet, which was a high-protein diet, and their Mediterranean diet was not significant. It did not approach statistical significance. And yet they mentioned it anyway.
I was listening to National Public Radio today. The short report that they broadcast said that the inflammatory markers were higher on the low-carb, high-fat diet, and so that’s why the Mediterranean diet wins. The idea that C-Reactive Protein differences between the three diets wasn’t mentioned in the national report in that group. I haven’t seen that mentioned in the way that you’re mentioning it now. You have a concern that the data were trumpeted in some ways that they didn’t deserve ?
RON ROSEDALE: It was spun and twisted in a way to make their type of Mediterranean diet look beneficial compared to the very low-carbohydrate diet, which in fact their own data showed had considerably, significantly better metabolic results.
Do you think that if I talked with somebody who is an expert and a fan of high-carb, low-fat diets, say Dean Ornisch, for instance, do you think he would have some gripes about how they did the study?
RON ROSEDALE: It very well could be. I don’t know.
I don’t know either, but I’m curious whether someone who has an expertise there could look at this and say whether they felt like the low-fat, high-carb diets were fairly represented. I even find myself wondering whether or not the Harvard group could have invited an expert like you or Steve Phinney or Eric Westman to check how they were doing the high-fat, low-carb protocol to see if it was OK. It’s puzzling to me why your views are so different from the kind of diet that they chose.
RON ROSEDALE: That’s a great question. I think I’ve tried to maybe not be so politically correct in saying why that would be. I think one finds all too often a lack of true wonderment about scientific truths and instead studies are done more for marketing efforts than true science.
Let’s us do some wondering, then.
RON ROSEDALE: Great.
There were some other aspects of the hypotheses, the premises and the beliefs going into this study, that were interesting. This study began by saying that lots of people can lose weight, but very few people can maintain that weight loss, and one reason is because it’s hard to keep going when you have an unusual diet that’s supposed to be for your health and everyone around you is eating differently. But the other side of the premise was that people’s bodies change metabolically when they change how they eat, and the ways that their bodies change metabolically and with hormone signaling fight against them being able to keep the weight off. Do you think that’s true?
RON ROSEDALE: I think it is true short-term. But we know now that there are metabolic pathways that are instrumental in dictating what our wants and desires are as far as what we eat, what we burn, whether we burn fat or sugar and therefore whether we need to eat fat or sugar to sustain our energy requirements.
Do those metabolic pathways make a difference on whether we feel hungry or full or anxious or content with how we’ve been eating?
RON ROSEDALE: They dictate those things. They don’t just make an impact, they are those things. We know, for instance, that leptin is one of the major hormones, and there are multiple hormones that dictate hunger because of how important it is. Nature knows that the only way a person is not going to overeat is if they’re not hungry. We know now that one of the major defects in metabolism that causes people to overeat is because leptin is not being heard properly, i.e., leptin resistance. I strongly believe that leptin resistance is caused from spikes in leptin secondary to what people have been eating for years causing a down-regulation in the ability of the brain and the hypothalamus in particular to listen to what leptin is trying to say, such that if a person has too much leptin, where normally it would reduce hunger and increase the ability to burn fat, the brain is hearing a different message. It’s hearing too little leptin, even though there’s a lot of it, and thinking that the person might be starving and therefore will increase their hunger and prevent the ability to burn fat properly.
So there’s a disregulation in leptin signaling which we know occurs in almost all overweight and obese people. And the way to correct it, I’ve found, at least 15 years ago now, I think I wrote one of the first books, maybe the first book on leptin and its clinical application to disease, is that you have to eat to maintain a low leptin, and the lower the leptin, the greater the signal. Just like we know that if a person eats appropriately, insulin levels will go down, their serum insulin will go down along with their blood sugar, so that we know that insulin is being heard better and you can alleviate the vast majority of cases of type 2 diabetes by eating a diet that is very low in carbohydrate, not high-protein, just enough protein to meet your needs, which is normally between 50 and 70 grams a day, depending on your size and activity level, and that will keep both insulin and leptin down and improve their signaling.
So even though the levels are coming down, the power of the signal is increasing, and therefore hunger will go down, the person will eat less long-term and they will burn more fat. And that’s really what this study showed. They just don’t want to admit it.
Hunger and Weight Maintenance
One of the premises of this study has been that it’s hard to do prevent hunger from getting out of control, and so people gain weight back. The study hints that it may not be as hard as they thought, but the idea that it’s hard to maintain your weight once your leptin levels have been high and then they go down, that comes from the 1990s, maybe early 2000s, where Rudy Leibel and Michael Rosenbaum out of Columbia had studies of leptin where they believe that they showed very consistently that once somebody has been fat and overweight or obese, if they lose weight, that leptin signal is always going to haunt them and push them to have their weight go back up again.
RON ROSEDALE: That’s correct, unless you eat a diet that will consistently keep leptin low and you go through a transformation period of several weeks that increases leptin sensitivity. I’m well aware of their study, and they are very wrong in their conclusion, just like this paper was.
You may believe that they’re very wrong, but their conclusions are governing nutritional policy in the U.S.
RON ROSEDALE: Which is why we are seeing a record number of obese and diabetic people around the world.
Maybe I should call them up and ask them some questions about whether in their studies they ever put someone on a truly high-fat, low-carb, adequate-protein diet after they had lost weight to see if then they would maintain their weight.
RON ROSEDALE: That would be great, and I think they will say they haven’t, because if they did, they would have seen exactly what I have seen for the last 20 years, that weight loss can usually be maintained, and that maintenance is almost parallel to leptin and insulin levels.
I did talk with one of those scientists many years ago and I think I remember him saying that when people were losing weight, they weren’t hungry, but once they had to be maintaining weight, their hunger came back.
RON ROSEDALE: And they were “maintaining” their research subjects on a higher-carbohydrate diet.
So when their test subjects were losing weight, they were basically burning their own body fat, so that they were on a high-fat diet.
RON ROSEDALE: They were burning their body fat and their muscle because they weren’t really putting them on a proper diet. They were putting them on a high-carbohydrate diet that maintained their essentially addiction to burning sugar as a primary fuel. One of the things I’ve said many, many times and really, I think, should dictate all health and nutrition policy, is that the person’s health and longevity is going to be determined by the proportion of fat versus sugar they burn over a lifetime. The more fat you burn, the healthier you’ll be. The more sugar you have to burn, the more unhealthy you’ll be. And that’s your choice in fuels. You can burn sugar or you can burn fat or byproducts of fat metabolism called ketones. If you burn fat and ketones, you’re going to be healthy.
Whether you burn fat and ketones is going to be dictated by hormones, such as leptin and insulin. And those hormones, in turn, are dictated by what you eat. So you have to eat to regulate the hormones that regulate whether you burn fat or sugar, and that in turn will dictate health.
That’s a good thing for people to remember, a helpful thing if they want to try a high-fat, low-carb diet and reasons to stay with it.
Is a Higher Metabolic Rate Healthy?
Getting back to the study, one of its premises is that it’s not a good thing when people lose weight and their metabolism goes down because if their metabolism goes down, it doesn’t take as many calories for them to maintain their body. So one of the measures that this study used for whether people were having a diet that worked for them is whether their metabolism stayed revved up. What do you think about that?
RON ROSEDALE: I think that really shows an ignorance of metabolism. I hate to put it that way, but it’s true. Again, in calorie-restricted animals and centenarians, one of the few commonalities that is very powerful is that free T3, the active thyroid, goes down, as does body temperature. In other words, the body goes into a more thrifty state so that it can maintain itself longer and healthier.
So the metabolism goes down?
RON ROSEDALE: It goes down because it’s healthier. It’s not metabolism going up or down, really, that is even relevant. It’s the quality of metabolism rather than the quantity of metabolism. For instance, on a person’s car, you can increase so-called thermogenesis, the metabolism of your car, as indicated by the standing RPMs. In other words, you’re at a stop sign. Would you want high RPMs or low RPMs? You want lower RPMs that are nice and smooth. So let’s say you’re at a stop sign and your car is running rough and it’s stalling out on you. You can go to a shop and one thing they could do is increase the metabolism of your car by increasing the baseline RPMs. In other words, instead of 600 they might put it to 1,000 or 1,200, so that it’s revving high.
What you’ll notice on your car, then, is that the temperature of the car, of the engine, will be hotter. It’s increasing thermogenesis. It’s increasing its heat output.
Does it also mean that it would take more gas to have it go the same amount of miles?
 RON ROSEDALE: It will take more gas to go the same amount of miles, which burns it out, but it also gets far less mileage. So the longevity of the engine will go way down. The mileage, which will dictate basically how long that car is going to live, will go way down. The pick-up of the car, even, will go down. So even though the metabolism is up, the useful energy of that car goes down. And that’s not what we want.
RON ROSEDALE: It will take more gas to go the same amount of miles, which burns it out, but it also gets far less mileage. So the longevity of the engine will go way down. The mileage, which will dictate basically how long that car is going to live, will go way down. The pick-up of the car, even, will go down. So even though the metabolism is up, the useful energy of that car goes down. And that’s not what we want.
That’s true. I don’t buy a car because I want it to take more gas to get the same amount of miles, and I don’t buy a car because it’s going to burn out faster.
RON ROSEDALE: No. Most people wouldn’t. In fact, if a person was pulling into a gas station and they could get one of two fuels, and on one gas tank it said, “This gas will cause your car to run hotter and get less gas mileage,” as opposed to the other tank that will say, “This will cause your car to run cooler,” in other words, lower metabolism, “and get better mileage,” which do you think people would get? They would always get the one that gets better mileage and causes their car to run cooler, because they know that’s better.
We operate under the exact same laws of physics. There’s no difference. Science in science. It permeates everything, including humans. And it amazes me how people can go to a health food store and how comments as in this paper talking about increasing metabolism as if it’s a good thing, and then have actually zero knowledge about the baseline science behind it.
It’s often said that it’s a good thing about a diet if it keeps your metabolism revved up, and it’s a bad thing to have metabolism go down. And here you are saying that having some of these indicators of how hot your body is running go down actually means that your body’s just running better.
RON ROSEDALE: Exactly correct. There’s so much misinformation and myth out there in health and nutrition and medicine in general. This is not new information. I’ve been saying the same thing for 20 years, and one of these days, hopefully the message will get through. I just hope I’m alive to see it.
Here you are where you and Eric Westman and Steve Phinney and Jeff Volek see the same way on protein now. That’s something that has evolved over time. I think it was Isaac Asimov, the science fiction writer, who pointed out that the world really is sort of flat, because it’s only a tiny bit round. But that small degree of roundness is enough to make the whole world round. It’s taken time to take all of those different ideas about roundness and flatness to refine them into what our world looks like. Maybe it’s the same way with nutrition.
RON ROSEDALE: Certainly we hope so. The major problem these days, which is quite different from Isaac Asimov’s time, is that knowledge now can be disseminated very easily. There’s no excuse to not be up to date. All you have to do is go on the Internet, and read. The problem is that there is less of a motive to actually learn science as there is a profit motive. That’s the major impediment to the advancement of science. It’s really unfortunate.
I’m not making any money by talking with you, and I don’t know that you’re making any money by talking with me, so let’s ask another question of wonderment. You said that having a metabolism be revved up just to make it hotter is not so good. But sometimes metabolism can go up for good reasons, and since you were talking about cars, I’m picturing the difference between a car that is running efficiently on the fuel that it has and getting lots of miles to the gallon and a car that doesn’t use a lot of gallons of gas because it’s too sluggish to run at all. I guess that that kind of slow metabolism in a car is not a good, healthy metabolism. Is there a kind of metabolism that could be measured in people where it indicates that their bodies are efficient, but also that their bodies have access to energy and can use it?
RON ROSEDALE: Definitely. Certainly if your metabolism is very low, and probably it’s at its lowest point when you die, that obviously wouldn’t be good, it would be one extreme. What you want, basically, as I mentioned, is the ability to burn fat. That can be easily determined by many different laboratory parameters. You can measure insulin, leptin, blood glucose, thyroid, especially free T3 or reverse T3, which actually should go up. It’s another misconception that reverse T3 indicates a disease state. It does not. It’s one of the ways that your body has of regulating thyroid activity.
There are many different metabolic markers that can be measured to indicate a healthy metabolism as opposed to a deranged metabolism that is unable to perform. The difference is, for instance, there’s a lot of misconceptions about thyroid. We know in calorie-restricted animals and in very low-carbohydrate diets, in the vast majority of modalities that increase lifespan and health in laboratory animals, the active thyroid, free T3, goes down. So many people use that as an excuse, really, or a reason that very low-carbohydrate diets are detrimental, saying that it causes hypothyroidism. And again, that’s really misguided knowledge. That’s not hypothyroid. The TSH, thyroid-stimulating hormone, from the pituitary does not go up. In other words, it’s a purposeful down-regulation of thyroid to allow the body to run in a healthier, more beneficial state, not because it has to, but because it wants to.
Whereas in hypothyroidism, what you’ll see is the body trying to make more thyroid but it can’t. So the TSH is high while active thyroid is low. That’s a big difference if your body wants higher thyroid but can’t do it, as opposed to the body purposefully lowering the thyroid because it’s healthier to do so.
Want versus can’t. That’s a pretty big difference. You’re implying that when it comes to the metabolism of a person, if a person’s body is running hot all the time, that’s different from a body where when a body needs to get extra energy it can. Going back to the study, do you think the higher metabolic rate of the people on the high-fat, low-carb diet was because their bodies were running better or because they had too much protein increasing the metabolism?
RON ROSEDALE: One of them definitely had to do with the protein content. We know that protein is very thermogenic. It’s unhealthy, and the body will essentially be forced to burn excess protein, and in this particular case there were probably 100 grams of excess protein a day, which is a huge amount. That’s number one. Number two is that leptin went down considerably, more in the very low-carbohydrate diet, even with the high protein. It would have gone down further, I believe, if it hadn’t been a high-protein diet. But even with the high-protein, very low-carbohydrate diet, leptin went down the most. When it goes down over time, it improves the signaling and it improves leptin sensitivity, which will allow your body to want to start burning off excess fat. It’ll notice then, “Whoa! We’ve got way too much fat to be healthy.” In our ancestral times, carrying around extra fat would be a death sentence, because any animal chasing a group of people would go after the fattest one that couldn’t make it up the tree, and also the fat person wouldn’t be able to hunt and gather very well to even feed themselves.
So being fat in our ancestral history was very disadvantageous. Your body doesn’t want you to be fat. One of the major regulatory methods that the body has to keep a person healthy and prevent fatness is proper leptin signaling. So by going on a very low-carbohydrate diet that does lower leptin more than any of the other diets, even in this study, you improve leptin sensitivity, so you actually improve the signaling more, and you’ll end up burning more fat, which will at least temporarily, until you burn off the excess fat, increase your metabolism, if you want to look at it as such.
Then are you glad this study measured leptin?
RON ROSEDALE: Yes, I’m glad it measured leptin. I’m glad it measured insulin and glucose and some of the other metabolic markers. It would have been quite a travesty had it not.
So there are some things that you’re glad they did in this study, but there are some areas where you have questions. I will see if I can ask some of these questions and share with you the answers when I get them.
RON ROSEDALE: That would be great. As I say, it wasn’t a bad study per se. I think the conclusions that were drawn were a bit misguided, and I think what they were trying to do is essentially reach for straws to try to support a diet that they’ve been supporting now for years.
And you have some wishes that they had done a little bit different choices in the study, for instance, how they measure cortisol is a big one, and the timing of when they measured C-reactive protein also so that they could see whether there were changes over time. And you sure wish that they hadn’t used so much protein for the high-fat, low-carb branch of the study.
RON ROSEDALE: That would have been, I think, far superior. For instance, on the CRP, had they just been looking at it from an objective standpoint and not trying to support one diet over another, all they would have said was that there was no statistically significant difference. If you’re going to use statistical significance the way it’s typically done in these studies, you can’t use it for certain parameters and not for others.
If you ever do a study of a high-fat, low-carb, adequate-protein diet, do you think you’d like to invite these researchers that like the Mediterranean diet to look over your shoulder so that they can give some input ahead of time?
RON ROSEDALE: You really want the truth on that?
[laughs] Sure!
RON ROSEDALE: The real truth is, no, because I know that they don’t know a tiny fraction of what I know about metabolism. I don’t think there’s any input that they could give me that would be worthwhile.
I’m thinking in terms of how if you have a lot of people looking at the elephant from their different perspectives, if they talk about it first to say what they’re looking for and how to sketch in the picture, it does sound like, from your perspective, the Harvard group overlooked some obvious things on how to make this be a better study. And whether that was intentional or not is hard to say.
RON ROSEDALE: I think not only did they overlook some things as far as what they measured, but I think the biggest detriment was the perhaps lack of knowledge in interpreting the data. Perhaps they don’t know that high cortisol is not necessarily bad but in fact is seen in centenarians and calorie-restricted animals and is actually viewed by many as one of the reasons that they live longer, due to its anti-inflammatory effect. So either they didn’t know that, or they purposely ignored that, which is something that shouldn’t have been done.
I’ll look forward to talking with them.
Thanks to Sandy Grabowski for the transcription. sandy (@) csd.net












6 comments for “Ron Rosedale Comments on New Harvard Study”